I suffer from pain that increases every time I do some strenuous activity and am afraid of harming myself. What to do?
The most important thing to do when you have chronic pain is to move. Normal movement of the body will not cause damage, but lack of movement will perpetuate the pain. Lack of movement leads to muscle wasting, calcium leakage, increased blood pressure and blood sugar levels and depression. Alongside the treatment for the pain, one should try and maintain as much as possible normal day-to-day conduct. It is recommended to start with gentle movements, easy general function and progress slowly. A good recommendation is to start with QiGong exercises) and maybe after that move to “Tai Chi”. Swimming can help a lot (in the elderly, it is often better to avoid breaststroke).
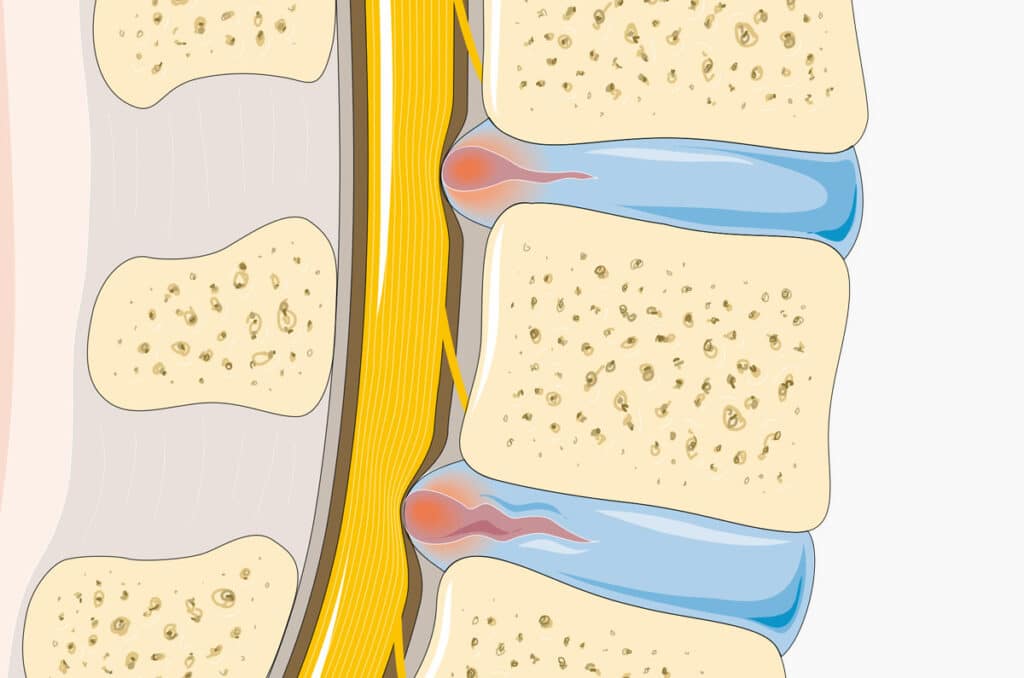
I have had lower back pain radiating down my leg for years. Some doctors recommend I have an epidural injection and others have recommended that I do surgery. What should I do?
As with most cases of chronic pain, there are likely to be multiple causes of chronic pain at the same time. If there is prolonged pain in the lower back, the pelvic joints absorb excessive loads that also pass through the hip joints and buttock muscles; Any of these structures may be contributing to your pain. There are situations where the patient has 3-4 causes of pain at the same time and it is difficult to define which one causes your pain. In the treatment of chronic pain, all possible factors must be taken into account. A doctor who has a very thorough approach both in taking an anamnesis and in a physical examination must evaluate you before you make any decision.
Chronic pain
From a personal perspective, any pain is troublesome. From a medical standpoint, we differentiate between 2 main types of pain, acute and chronic. Chronic pain is defined as pain that lingers on for more than 3 months whereas acute pain usually resolved within a few weeks.
Chronic pain can arise from several causes such as accidents, falls, ligament and tendon injuries, fractures which don’t heal, spinal pathology or faulty ergonomics. Sometimes, several pathologies, sometimes up to 3-4, can coexist. For example, if there is damage to a structure in the knee, the patients will bear more weight on the opposite leg. Treatment of chronic pain must address all causes of pain in order to achieve long-lasting results.
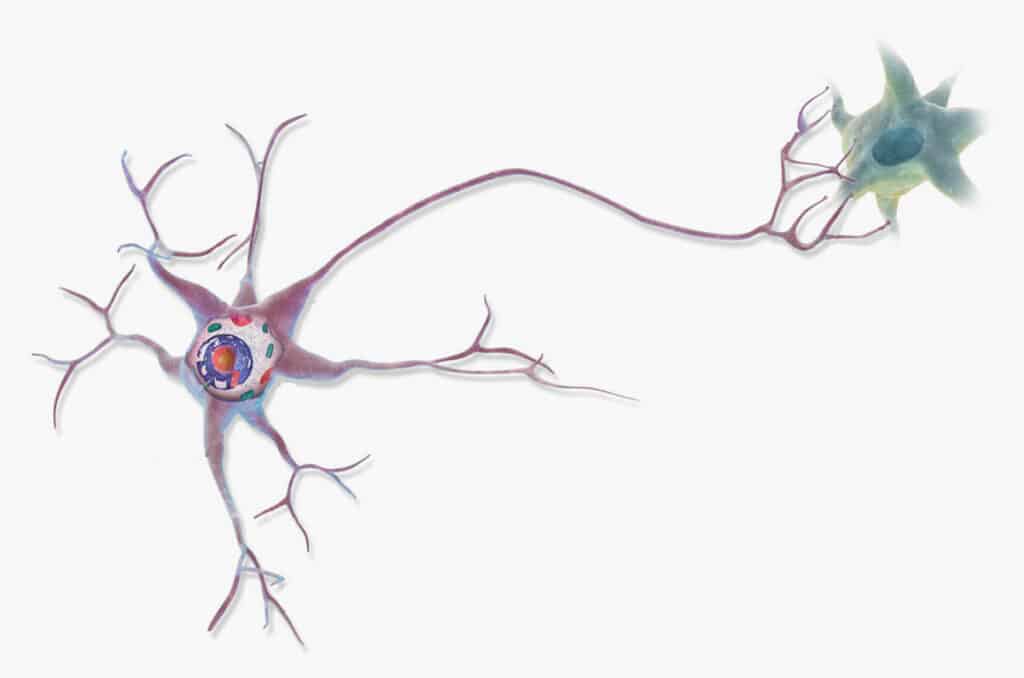
Acute pain has an important role to play; it warns us against impending danger such as fire or a sharp knife. Chronic pain, however, has no clear purpose. In addition, there is little connection between the severity of chronic pain and of tissue damage. Often a significant injury occurs to a patient who feels little pain and often the reverse is very common as well. There are those with advanced cartilage degeneration or a severe disc prolapse though the patient feels almost no pain. And there are those with minimal damage but are bedridden and don’t function at all.
Chronic pain affects our mood and sleep, both of which in turn will increase the pain and hence create a vicious cycle.
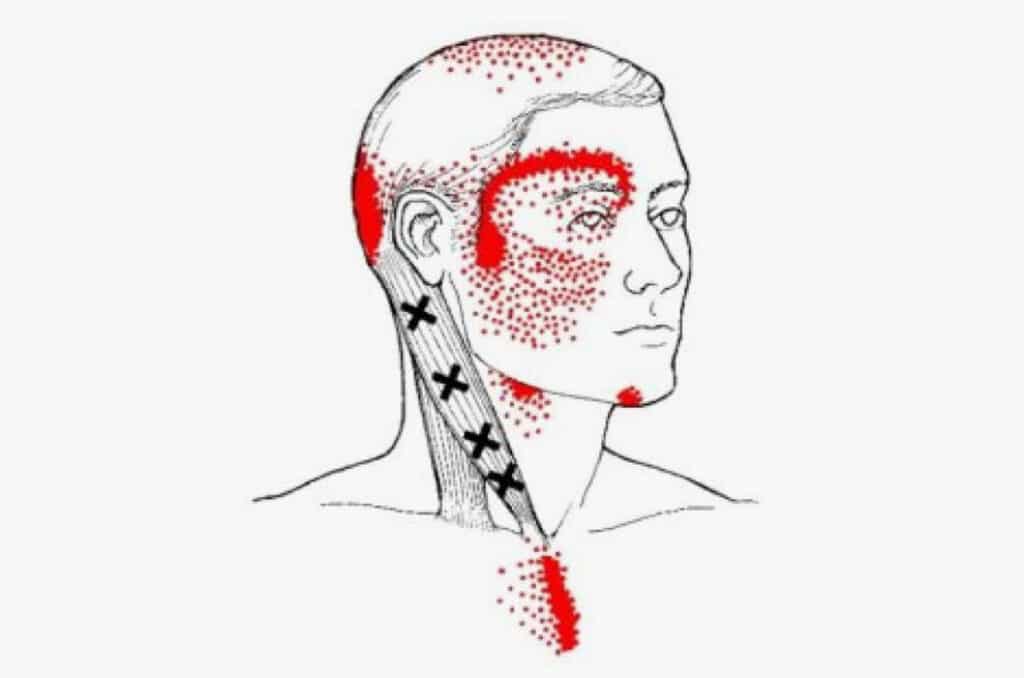
Treatment of chronic pain must be based on an understanding of the cause, musculoskeletal dysfunction, improper ergonomics as well as emotional factors which react to yet may also add to the pain. If the problem is of musculoskeletal origin, one can be treated with a combination of various treatments including dry needling, prolotherapy and platelet-rich plasma injections. If the problem arises from a neural source, epidural injections or nerve hydrodissection blocks can be performed with various injectates.
The neural pathways relaying emotions between the brainstem and the brain run in common pathways relaying pain sensation, therefore negative emotions can potentially perpetuate the pain. It is a physiological process and one cannot deny it. Failure to treat this emotional component will often lead to failure to treat the pain. Conversely, studies have shown the laughter reduces cortisol levels in the bloodstream and consequently reduces pain. So keep happy, watch comedies. It is for these reasons that a doctor may request to combine psychological therapy, such as cognitive behavioural therapy or hypnosis with other treatments.
The bottom line of any treatment- KEEP MOVING! And of course, keep happy.